Available in TCP Vol. 76, Issue 2
By Ateka A. Contractor, Anne N. Banducci, & Andrea Fentem
Trauma is a common experience, with ~90% of individuals in the United States and ~70% of individuals across 24 countries reporting a traumatic experience in their lifetime (Benjet et al., 2015; Kilpatrick et al., 2013). Trauma exposure takes a toll on societies and individuals, leading to the development of posttraumatic stress disorder (PTSD) for a sizable minority of individuals (Magruder et al., 2017). PTSD is characterized by intrusive thoughts and trauma-related memories, avoidance of trauma-related triggers, maladaptive changes in thinking and affective processes, and alterations in arousal and reactivity (American Psychiatric Association, 2013). Substantial observational, experimental, and neurobiological research suggests that the experience of a trauma and PTSD entails disruptions in several aspects of both traumatic and positive autobiographical memories, including the capacity to learn information, the content of memories, as well as memory processes such as encoding, storage, and retrieval (e.g., Bomyea et al., 2017; Brewin & Holmes, 2003; Contractor et al., 2018; Kida, 2019; Ono et al., 2016; van Marle, 2015). As such, intervening on memory-related processes has been a key focus when treating PTSD.
Untreated PTSD has been linked to indicators of functional impairment and economic burden, such as social problems (e.g., difficulties in interpersonal relationships; Riggs et al., 1998), physical health problems (e.g., cardio-respiratory symptoms; Pacella et al., 2013), psychological problems (e.g., depression; Jacobson et al., 2001; Rytwinski et al., 2013), and financial costs to society (Kessler, 2000). Thus, providing effective preventive care and clinical interventions to individuals who are struggling with PTSD symptoms is imperative. Trauma-focused therapies, which are generally efficacious, are the gold standard treatment for PTSD (Schnurr, 2017). There is room for improvement, however, given ~34-56% of trauma-focused treatment recipients do not experience remission following treatment (Cusack et al., 2016; Schnurr, 2017) and a substantial proportion of individuals discontinue treatment prematurely (Garcia et al., 2011; Hembree et al., 2003). Such treatment non-response and dropout may be attributed to memory-related processes, such as broader difficulties with trauma memory retrieval and the anticipated fear of anxiety-related sensations during exposure to trauma memories (Belleau et al., 2017; Leiner et al., 2012; Schottenbauer et al., 2008). Although modifying existing strategies (e.g., massed treatments for trauma-focused interventions) to increase successful engagement and retention in these trauma-focused treatments is critical, it is also important to consider novel strategies to address PTSD, in order to have a broader range of effective treatment options for trauma survivors. In this regard, a relatively unexplored and promising target is processing positive memories. In this manuscript, we will discuss evidence that supports addressing positive memories in PTSD interventions, as well as future directions for this line of work.
Why Should We Address Positive Autobiographical Memories in PTSD Interventions?
First, positive autobiographical memories have characteristics that individuals find appealing, valuable, and beneficial. Generally, positive memories are central to individuals’ identities, life stories, and belief structures across cultures (Foley, 2018; Zaragoza Scherman et al., 2015a), are highly accessible and arise frequently (Walker et al., 2003; Williams et al., 2022), and are favored over time (Matlin & Stang, 1978). Further, retrieval of one positive memory increases the likelihood of retrieving other positive memories, and the affect experienced when recalling positive memories tends to remain for a substantial period of time (Ritchie et al., 2009; Williams et al., 2022). Thus, discussing positive memories in a therapeutic setting may be appealing and beneficial to clients.
Second, trauma survivors with PTSD symptoms experience difficulties retrieving both specific traumatic and positive autobiographical memories. Indeed, a recently published scoping review concluded that individuals with PTSD generally retrieve fewer specific positive autobiographical memories compared to individuals without PTSD, and that individuals with experiences of childhood interpersonal traumas retrieve fewer specific positive autobiographical memories (Contractor, Caldas, Dolan, et al., 2022). Regarding PTSD symptom clusters, in a study of 203 trauma-exposed community participants, more PTSD symptom cluster severity (i.e., intrusions, negative alterations in cognitions/mood, and alterations in arousal and reactivity) was associated with fewer retrieved specific positive autobiographical memories (Contractor et al., 2019). Given this research, the question of concern is—why do trauma survivors with PTSD symptoms have deficits with positive memory processes? Consistent with the scarring hypothesis (Williams et al., 2007), trauma memories and related negative content become central to trauma survivors’ identities, and consequently, these individuals find it difficult to retrieve specific positive autobiographical memories and to integrate these memories with other lifetime memories (Bernsten & Rubin, 2007; Brewin et al., 2010; Brewin & Holmes, 2003). Additionally, these individuals may experience a wide range of negative emotions and less positive affect when reflecting on memories of past events (Clifford et al., 2020), may not be able to effectively regulate the positive emotions they experience when retrieving positive autobiographical memories (Contractor, Weiss, & Forkus, 2021), and may retrieve over-general memories of past events to cope with posttraumatic distress (Moore & Zoellner, 2007). Such patterns may contribute to less retrieval of specific positive autobiographical memories. Conversely, the vulnerability hypothesis suggests that difficulties retrieving specific positive autobiographical memories may increase the likelihood of experiencing distress after a trauma (Williams et al., 2007). Examples of such vulnerability factors include fewer pre-trauma positive experiences and their associated memories, and difficulties accessing pre-trauma positive memories (Bryant et al., 2007; Hauer et al., 2009). In sum, a variety of processes decrease the likelihood of trauma survivors with PTSD symptoms effectively retrieving and engaging with specific positive autobiographical memories, pointing to the necessity of intervening in this area.
Third, cross-sectional evidence links positive autobiographical memory processes and characteristics to PTSD symptoms. For instance, in a sample of 185 trauma-exposed community participants, those with greater PTSD symptom severity reported less vividness of, less coherence of, less accessibility to, fewer temporal/sensory details of, and more distancing from retrieved positive memories (Dolan et al., 2020). Acknowledging the heterogeneity embedded in the construct of PTSD, we have also examined particular PTSD symptom clusters in relation to positive autobiographical memory processes and characteristics. In a community sample of 206 trauma-exposed individuals, those with more severe PTSD arousal symptoms reported fewer positive autobiographical memories, as well as less positive autobiographical memory coherence and accessibility; and those with more severe PTSD avoidance symptoms reported fewer positive autobiographical memories (Contractor, Greene, et al., 2020). Separately, those with more severe PTSD negative cognitions/mood symptoms and arousal symptoms reported less accessibility to positive autobiographical memories (Contractor et al., 2019). Such research is also supported by longitudinal evidence, which we elaborate below.
Lastly, observational and experimental longitudinal evidence links positive autobiographical memory processes and characteristics to PTSD symptoms. For instance, in a sample of 238 trauma-exposed students completing daily assessments for 10 days, there was a bidirectional relationship between PTSD symptom severity and positive memory characteristics. On days where students experienced more severe PTSD symptoms, their positive memories were less vivid and accessible, and vice versa (Contractor, Messman, et al., 2022). Interestingly, there were no lagged associations; PTSD symptom severity or positive memory vividness and accessibility reported on a prior day were not associated with positive memory vividness and accessibility or PTSD symptom severity, respectively, the following day (Contractor, Messman, et al., 2022). In a separate sample of 74 women reporting intimate partner violence and substance use, approximately 50% of the surveyed women with more severe PTSD symptoms reported less positive memory vividness and accessibility. Notably and not as expected, approximately 50% of the surveyed women with more severe PTSD symptoms reported more positive memory vividness and accessibility (Contractor, Natesan Batley, et al., in press).
In sum, cross-sectional and longitudinal research using diverse methodologies from our laboratory suggests that trauma survivors with PTSD symptoms report difficulties accessing and retrieving specific and detailed positive autobiographical memories. However, there is some heterogeneity, wherein these patterns are not true for all trauma survivors. We have only examined a few contextual factors that explain this divergence. In this regard, our research suggests that presence of sleep disturbances as well as one’s ability to regulate positive emotions may influence relations between PTSD symptoms and positive autobiographical memories (Contractor, Slavish, et al., 2021; Contractor, Weiss, & Forkus, 2021). Future research would benefit from exploring person-specific and environmental factors impacting the retrieval of positive memories in trauma survivors’ daily lives and within therapeutic settings.
Positive Memory-PTSD Model and Processing of Positive Memories Technique for PTSD
Given the aforementioned research, our group has continued to explore why trauma survivors with PTSD symptoms have difficulties retrieving positive autobiographical memories and how we can intervene using positive memory processes as therapeutic targets, to expand our options for ameliorating PTSD symptomatology effectively. Such efforts led to the development of an overarching theory explaining these processes, the Positive Memory-PTSD Model, as well as to the development of an intervention targeting these positive autobiographical memory processes, the Processing of Positive Memories Technique for PTSD.
The Positive Memory-PTSD Model integrates findings from experimental evidence, memory intervention research, and positive psychology intervention research (Contractor, Banducci, et al., 2022; 2018). See Figure 1 for diagrammatic representation of the Positive Memory-PTSD Model. 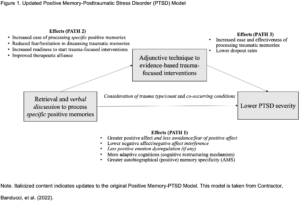 Our model suggests that the retrieval and processing of specific positive memories may improve PTSD symptoms, affect, and beliefs, as well as facilitate benefits for subsequent trauma-focused treatments (e.g., enhanced readiness to start trauma-focused treatments, less likelihood of dropping out from trauma-focused treatments; Contractor et al., 2018). This Positive Memory-PTSD Model spurred further research in the area of PTSD and positive memories, which was important because the majority of prior positive memory intervention work has been in the area of depression. Indeed, scoping reviews, systematic reviews, and meta-analyses demonstrate that positive memory processing generally has the greatest impact on improving positive affect and on reducing depressive symptoms (see Hitchcock et al., 2017; Miguel-Alvaro et al., 2021). Further, Hitchcock and colleagues’ (2017) systematic review and meta-analysis found only one study focused on PTSD; the study compared a therapeutic technique addressing the retrieval of specific memories to a wait-list control, with results indicating larger decreases in PTSD symptoms in the intervention group. Hitchcock and colleagues (2017) concluded that while there is promising evidence for the beneficial impacts of memory-based interventions for depression, there is comparatively less research for PTSD, which hampers our ability to draw conclusions.
Our model suggests that the retrieval and processing of specific positive memories may improve PTSD symptoms, affect, and beliefs, as well as facilitate benefits for subsequent trauma-focused treatments (e.g., enhanced readiness to start trauma-focused treatments, less likelihood of dropping out from trauma-focused treatments; Contractor et al., 2018). This Positive Memory-PTSD Model spurred further research in the area of PTSD and positive memories, which was important because the majority of prior positive memory intervention work has been in the area of depression. Indeed, scoping reviews, systematic reviews, and meta-analyses demonstrate that positive memory processing generally has the greatest impact on improving positive affect and on reducing depressive symptoms (see Hitchcock et al., 2017; Miguel-Alvaro et al., 2021). Further, Hitchcock and colleagues’ (2017) systematic review and meta-analysis found only one study focused on PTSD; the study compared a therapeutic technique addressing the retrieval of specific memories to a wait-list control, with results indicating larger decreases in PTSD symptoms in the intervention group. Hitchcock and colleagues (2017) concluded that while there is promising evidence for the beneficial impacts of memory-based interventions for depression, there is comparatively less research for PTSD, which hampers our ability to draw conclusions.
Drawing from the Positive Memory-PTSD Model, we developed a novel 5-session Processing of Positive Memories Technique (PPMT), as a PTSD-specific intervention. This intervention aims to improve access to and the phenomenological quality of salient positive autobiographical memories, while capitalizing on the positive content from these memories (Contractor, Weiss, & Shea, 2021). PPMT was developed and refined using treatment development guidelines (Rounsaville et al., 2001) as well as stakeholder input from therapists (Contractor, Caldas, et al., 2020) and trauma survivors seeking therapeutic services (Banducci et al., in press; Caldas et al., 2020). The detailed session-by-session content of PPMT is outlined in Contractor, Weiss and Shea (2021). Briefly, in Session 1, individuals receive psychoeducation and an overview of PPMT’s rational and goals, and are assessed for psychological symptoms. In Session 2, individuals recall one salient and meaningful positive autobiographical memory, narrate that positive autobiographical memory in detail, and process that positive memory to elicit values, affect, strengths, and thoughts (VAST) related to that memory to increase their salience to one’s identity. Homework assignments include listening to an audio-recording of the narrated memory, completing a VAST log, and engaging in a values-consistent positive behavioral activity (e.g., spending time with family and friends). Engaging in positive behavioral activities may also help them create more positive memories. Sessions 3-5 involve the same procedure as Session 2; individuals process different positive autobiographical memories in each session. In Session 5, the therapist additionally reviews psychological symptoms and treatment progress. Individuals receiving PPMT improve in their ability to retrieve and process salient positive autobiographical memories over time, which helps them access/strengthen core positive values, affect, strengths, and thoughts (i.e., improving affective and cognitive processes), as well as increases awareness of positive information incompatible with trauma fear structures. Consequently, positive memories may replace trauma memories as reference points, influencing beliefs and life experiences. All such processes may contribute to improved PTSD symptoms (Contractor, Weiss, & Shea, 2021).
We conducted two pilot projects with PPMT. Using an experimental design, 65 trauma-exposed students were randomized to one of three conditions (narrating two specific positive autobiographical memories, writing about two specific positive autobiographical memories, a time-matched control) to determine the most effective strategy for processing positive memories, and to assess for the benefits of processing positive autobiographical memories. Students in the narrating condition reported significant decreases in PTSD symptom severity, negative post-trauma cognitions, and negative affect; as well as significant increases in positive affect across timepoints compared to those in the time-matched control condition (Contractor, Banducci, et al., 2020). Next, we piloted our PPMT intervention among 12 trauma-exposed individuals seeking services at a university psychology training clinic (Contractor, Jin, et al., in press; Contractor, Slavish, et al., in press). Using an idiographic statistical approach, we found the following: 9 participants reported statistically reliable changes for PTSD symptom severity (8 recovered/improved); 5 participants reported statistically reliable changes for positive affect levels (2 recovered/improved); 5 participants reported statistically reliable changes for positive emotion dysregulation (4 recovered); 9 participants reported statistically reliable changes for negative affect levels (8 recovered); and 9 participants reported statistically reliable changes for negative posttrauma cognitions (7 recovered/improved). These results suggest that PPMT differentially impacts varied posttrauma targets. For example, PPMT may help more with PTSD, negative affect, and negative posttrauma cognitions; and may have stronger effects on emotion regulation than on levels of positive affect.
In summary, PPMT, if supported in further clinical investigations, may add to the clinician’s tool-box of PTSD interventions. To further gauge the impacts and benefits of PPMT, studies comparing PPMT to a control condition and with larger sample sizes of individuals diagnosed with PTSD is necessary. Emerging research suggests that targeting both positive and traumatic autobiographical memories improves PTSD symptoms (Hitchcock et al., 2017); with data suggesting that exclusively targeting positive autobiographical memories improves PTSD symptoms (Contractor, Banducci, et al., 2020; Miguel-Alvaro et al., 2021). Indeed, parallel to our work, Moradi and colleagues (2021) compared the effects of MemFlex (an intervention targeting the retrieval and elaboration of positive memories to improve individuals’ abilities to move between specific and general levels of memory representation) to a control condition among 43 Iranian trauma survivors. They found lower PTSD symptom severity at follow-up in the MemFlex group compared to the control condition. Together, we can situate PPMT within the context of other positive psychology and memory-based interventions for posttrauma wellbeing, with broader findings suggesting these interventions benefit trauma survivors reporting PTSD symptomatology.
Conclusions and Future Directions
Taken together, a robust body of work indicates that experiencing trauma not only impacts how traumatic memories are stored and retrieved, but also impacts the storage and retrieval of memories across the affective spectrum, including positive autobiographical memories. In this same vein, engaging with positive autobiographical memories, among trauma survivors, shares some of the same benefits of engaging with traumatic memories. Although this body of work is promising, there are a number of additional questions to consider and areas of exploration that we discuss below. We consider the generalizability and effectiveness of PPMT across a variety of populations, potential mediators and moderators, and outline next steps for this line of research.
First, based on clinical observations and research findings, there are critical points warranting additional investigation when translating PPMT for use among individuals with diagnostic PTSD. When we began doing this research, we did not expect that some individuals’ difficulties engaging with traumatic autobiographical memories would be mirrored by the same level of difficulties engaging with positive autobiographical memories. Yet, in our PPMT pilot studies, we noticed that some trauma survivors found it extremely challenging to identify and recall a specific positive autobiographical memory that defined them, was meaningful to them, and related to their outlook on life (Banducci et al., in press; Fondren et al., 2022). These individuals also found it difficult to provide details of positive autobiographical memories (Fondren et al., 2022). We also found that even if trauma survivors were able to provide details of specific positive autobiographical memories, it was difficult for some of them to remain focused on positive aspects of their memories, to be non-judgmental of themselves or their experiences, to be fully engaged with their positive autobiographical memories, or to be comfortable with allowing themselves to have pleasant emotions and thoughts when discussing the memory (Fondren et al., 2022). Such processes could be even more challenging for individuals with diagnostic PTSD, paralleling difficulties retrieving traumatic memories observed in prior work. For example, trauma survivors, especially those with diagnostic PTSD, who experience dissociation also report broader difficulties with their memory recall (Özdemir et al., 2015). Given this, it is critical to test PPMT among individuals with more severe posttrauma symptomatology, so that we can examine their ability to engage effectively with PPMT and benefit from it, as well as to better understand how therapists can most effectively guide and engage these individuals through the intervention.
Second, factors implicated in traumatic memory processes may also be relevant for positive autobiographical memories. For example, sleep may impact consolidation of positive memories, given that it impacts this process for traumatic autobiographical memories (van Marle, 2015). Contextual and individual-level factors may also interface with the effects of PPMT. For instance, trauma and PTSD symptoms hamper neurocognitive abilities, such as attentional allocation, executive functioning, and memory processes (LaGarde et al., 2010), and these factors may impact positive memory retrieval in PPMT. It is possible that PTSD-specific symptoms may lead to difficulties with positive autobiographical memory retrieval; avoidance of trauma memories may generalize to avoidance of all past memories, negative alterations in mood and cognition may reduce the amount of pleasure experienced when thinking about positive autobiographical memories or may lead to beliefs about not deserving to feel good, and arousal symptoms may lead to physical sensations associated with happiness or excitement being experienced as aversive. Thus, further work is needed to understand how PTSD-specific symptoms versus broader difficulties with memory retrieval due to cognitive and other factors, may impact trauma survivors receiving PPMT.
Third, research needs to investigate the need and nature of cultural adaptations of PPMT. Indeed, memory function, content, and processes are shaped by cultural factors (Wang & Ross, 2007; Zaragoza Scherman et al., 2015b). For instance, individuals in collectivistic cultures are more likely to value and share positive autobiographical memories, which may then translate to collective memories that positively impact the community’s identity (Reese & Fivush, 2008) and enhance emotional/social bonds (Wang, 2008). Indeed, individuals who identify as Asians tend to connect their life stories with that of the larger collective, in line with their collectivistic values (Wang, 2008); and often recall collective memories that involve social activities (Wang & Conway, 2004), which may help them cope with shared traumas (Wang, 2008). Thus, whether PPMT has differential impacts across a variety of cultural groups, or needs to be culturally-adapted and validated, is an important area of empirical investigation. This is especially important because positive autobiographical memories are central to individuals’ identities and life stories across cultures (Zaragoza Scherman et al., 2015a) and represent culturally unbiased risk factors for PTSD (Jobson et al., 2016). Thus, positive memory processes may be a unique point of culturally responsive interventions.
Fourth, across our studies, affect processes did not explain or influence the effects of retrieving positive autobiographical memories on posttrauma health (Contractor, Caldas, Banducci, et al., 2022; Contractor, Slavish, et al., in press), which is surprising given that we expected changes in affect to explain reductions in PTSD symptoms among trauma survivors receiving PPMT (see review by Contractor, Banducci, et al., 2022; Contractor et al., 2018). Interestingly, dysregulation of positive emotions has been shown to moderate relations between PTSD symptom severity and number of retrieved positive memories (Contractor, Weiss, & Forkus, 2021), such that more severe PTSD symptoms are associated with retrieving fewer positive autobiographical memories among trauma survivors who report positive emotion dysregulation. The question to investigate next is how different trauma survivors react affectively to retrieving and processing positive autobiographical memories in daily life, and whether facets of affect (e.g., arousal, valence, reactions to experiencing intense emotions) are relevant when considering who, or how trauma survivors, benefit from PPMT. Also, perhaps other mechanistic targets may explain the beneficial effects of PPMT, such as decreases in PTSD-related avoidance symptoms (Caldas et al., 2022).
Lastly, when considering how or why intervening on positive autobiographical memory processes benefits some individuals, it is helpful to consider learning processes. Research substantiates targeting the reconsolidation phase of traumatic memories to more effectively intervene on PTSD (e.g., blocking reconsolidation of the traumatic memory, facilitating fear memory extinction; weakening the traumatic memory by competition from other stimuli; Kida, 2019; Kindt & van Emmerik, 2016; van Marle, 2015). Much of this work has been conducted using conditioned fear models in animals, but there is evidence these processes are shared by humans. Recent work has demonstrated that activating a positive autobiographical memory during reconsolidation of a fear memory reduces conditioned fear acutely and enduringly (Grella et al., 2022). Although our paradigm does not focus on activating positive autobiographical memories during retrieval of traumatic memories, this work does demonstrate the power of positive autobiographical memories in disrupting traumatic memories, suggesting the utility of continuing down this path. Given that PPMT broadly evidences benefits for posttrauma health, it is worthwhile to examine how the retrieval of salient positive autobiographical memories interfaces with the reconsolidation of traumatic memories. Another aspect to consider is how the physical impacts of traumatic experiences may influence learning and thereby memory processes. Specifically, trauma survivors may experience head injuries, such as traumatic brain injuries or concussions, which can affect memory processes (Glaesser et al., 2004). These individuals may need alternative learning processes to encode and retrieve positive autobiographical memories.
Taken together, research suggest benefits to engaging with positive autobiographical memories among trauma survivors, whereas experimental, self-report, and longitudinal data demonstrates that individuals with more severe PTSD symptoms have difficulties with this very task. Whether these difficulties with memory retrieval differ among trauma-exposed and trauma-naïve populations, as a function of memory type (e.g., positive versus traumatic memories), is less understood. Indeed, we do not know who has difficulties engaging with positive autobiographical memories, or precisely why these difficulties are present. It is possible that pre-trauma factors like resilience, or having a more positive outlook impacts how trauma survivors engage with pleasant autobiographical memories. Separately, factors that make it difficult for some individuals to retrieve traumatic memories may also lead to difficulties retrieving positive memories (e.g., avoidance, cognitive factors). Looking forward, there are a number of important next steps to consider when implementing PPMT and making it scalable. We are eager to determine how and for whom PPMT will provide the greatest benefits in symptom reduction and for treatment engagement. Further, we need to determine the magnitude of the effects of PPMT among individuals with diagnostic PTSD, and whether PPMT may function effectively as a stand-alone treatment for some trauma survivors versus as an adjunctive pre-treatment intervention for others who also need trauma-focused interventions. Broadly, our research and clinical work lays the foundation for more work on positive autobiographical memories in the context of PTSD.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Association.
Banducci, A. N., Fondren, A., Bocanegra, A., Crespo, M., & Contractor, A. A. (in press). Feedback on components, format, and feasibility of the Processing of Positive Memories Technique (PPMT). Journal of Nervous & Mental Disease.
Belleau, E. L., Chin, E. G., Wanklyn, S. G., Zambrano-Vazquez, L., Schumacher, J. A., & Coffey, S. F. (2017). Pre-treatment predictors of dropout from prolonged exposure therapy in patients with chronic posttraumatic stress disorder and comorbid substance use disorders. Behaviour Research and Therapy, 91, 43-50. https://doi.org/10.1016/j.brat.2017.01.011
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., & Alonso, J. (2015). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46, 327-343. https://doi.org/10.1017/S0033291715001981
Bernsten, D., & Rubin, D. C. (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21, 417-431. https://doi.org/10.1002/acp.1290
Bomyea, J., Johnson, A., & Lang, A. J. (2017). Information processing in PTSD: Evidence for biased attentional, interpretation, and memory processes. Psychopathology Review, 4, 218-243. https://doi.org/10.5127/pr.037214
Brewin, C. R., Gregory, J. D., Lipton, M., & Burgess, N. (2010). Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review, 117, 210-232. https://doi.org/10.1037/a0018113
Brewin, C. R., & Holmes, E. A. (2003). Psychological theories of posttraumatic stress disorder. Clinical Psychology Review, 23, 339-376. https://doi.org/10.1016/S0272-7358(03)00033-3
Bryant, R. A., Sutherland, K., & Guthrie, R. M. (2007). Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. Journal of Abnormal Psychology, 116, 837-841. https://doi.org/10.1037/0021-843X.116.4.837
Caldas, S. V., Fondren, A., Natesan Batley, P., & Contractor, A. A. (2022). Longitudinal relationships between posttraumatic stress disorder symptom clusters in response to positive memory processing. Journal of Behavior Therapy and Experimental Psychiatry, 76. https://doi.org/10.1016/j.jbtep.2022.101752
Caldas, S. V., Jin, L., Dolan, M., Dranger, P., & Contractor, A. A. (2020). An exploratory examination of client perspectives on a positive memory technique for PTSD. Journal of Nervous and Mental Disease, 208, 230-237. https://doi.org/10.1097/NMD.0000000000001082
Clifford, G., Hitchcock, C., & Dalgleish, T. (2020). Negative and positive emotional complexity in the autobiographical representations of sexual trauma survivors. Behaviour Research and Therapy,, 126. https://doi.org/10.1016/j.brat.2020.103551
Contractor, A. A., Banducci, A. N., Dolan, M., Keegan, F., & Weiss, N. H. (2019). Relation of positive memory recall count and accessibility with posttrauma mental health. Memory, 27, 1130-1143. https://doi.org/10.1080/09658211.2019.1628994
Contractor, A. A., Banducci, A. N., Jin, L., Keegan, F., & Weiss, N. H. (2020). Effects of processing positive memories on posttrauma mental health: A preliminary study in a non-clinical student sample. Journal of Behavior Therapy and Experimental Psychiatry, 66(101516). https://doi.org/10.1016/j.jbtep.2019.101516
Contractor, A. A., Banducci, A. N., & Weiss, N. H. (2022). Critical considerations for the Positive Memory-Posttraumatic Stress Disorder model. Clinical Psychology & Psychotherapy, 29(1), 81-91. https://doi.org/10.1002/jclp.23142
Contractor, A. A., Brown, L. A., Caldas, S., Banducci, A. N., Taylor, D. J., Armour, C., & Shea, M. T. (2018). Posttraumatic stress disorder and positive memories: Clinical considerations. Journal of Anxiety Disorders, 58, 22-32. https://doi.org/10.1016/j.janxdis.2018.06.007
Contractor, A. A., Caldas, S., Banducci, A. N., & Armour, C. (2022). A pilot study examining roles of cognitions and affect between positive memory processing and posttraumatic stress disorder severity. Psychological Trauma Theory Research Practice and Policy, 14, 661-668. https://doi.org/10.1037/tra0000625
Contractor, A. A., Caldas, S. V., Dolan, M., Banducci, A. N., & Jin, L. (2020). Exploratory examination of clinician perspectives on positive memories and posttraumatic stress disorder interventions. Counselling and Psychotherapy Research, 20, 92-105. https://doi.org/10.1002/capr.12267
Contractor, A. A., Caldas, S. V., Dolan, M., & Weiss, N. H. (2022). Factors related to positive memory count among trauma-exposed individuals: A scoping review. Trauma Violence Abuse, 23(5), 1568-1584. https://doi.org/10.1177/15248380211013130
Contractor, A. A., Greene, T., Dolan, M., Weiss, N. H., & Armour, C. (2020). Relation between PTSD clusters and positive memory characteristics: A network perspective. Journal of Anxiety Disorders, 69. https://doi.org/10.1016/j.janxdis.2019.102157
Contractor, A. A., Jin, L., & Weiss, N. H. (in press). Open label pilot study on posttrauma health impacts of the Processing of Positive Memories Technique (PPMT). Journal of Psychotherapy Integration.
Contractor, A. A., Messman, B. A., Slavish, D. C., & Weiss, N. H. (2022). Do positive memory characteristics influence daily-level trajectories of posttraumatic stress disorder symptoms? An exploratory daily diary study. Anxiety, Stress & Coping, 1-19. https://doi.org/10.1080/10615806.2022.2075856
Contractor, A. A., Natesan Batley, P., Compton, S. E., & Weiss, N. H. (in press). Relations between posttraumatic stress disorder symptoms and positive memory characteristics among women reporting intimate partner violence: A micro-longitudinal study. Journal of Interpersonal Violence.
Contractor, A. A., Slavish, D. C., Thornton, J., & Weiss, N. H. (in press). Positive affect processes and posttraumatic stress disorder symptoms: Findings from an open label and uncontrolled pilot study using the Positive Memory Processing Technique. Journal of Psychotherapy Integration.
Contractor, A. A., Slavish, D. C., Weiss, N. H., Alghraibeh, A. H., Alafnan, A. A., & Taylor, D. J. (2021). Moderating effects of sleep difficulties on relations between posttraumatic stress disorder symptoms and positive memory count. Journal of Clinical Psychology, 77, 2057-2076. https://doi.org/10.1002/jclp.23142
Contractor, A. A., Weiss, N. H., & Forkus, S. R. (2021). Moderating effects of dysregulation and fear of positive emotions on the relationship between posttraumatic stress disorder symptoms and positive memory count. Journal of Clinical Psychology, 77, 701-721. https://doi.org/10.1002/jclp.23046
Contractor, A. A., Weiss, N. H., & Shea, M. T. (2021). Processing of Positive Memories Technique (PPMT) for posttraumatic stress disorder: A primer. Journal of Psychotherapy Integration, 31, 195-207. https://doi.org/10.1037/int0000239
Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., Feltner, C., Brownley, K. A., Olmsted, K. R., Greenblatt, A., Weil, A., & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychological Review, 43, 128-141. https://doi.org/10.1016/j.cpr.2015.10.003
Dolan, M., Contractor, A. A., Ryals, A., & Weiss, N. H. (2020). Trauma, posttraumatic stress disorder severity, and positive memories. Memory, 28, 998-1013. https://doi.org/10.1080/09658211.2020.1809679
Foley, M. A. (2018). Reflecting on how we remember the personal past: Missing components in the study of memory appraisal and theoretical implications. Memory, 26, 634–652. https://doi.org/10.1080/09658211.2017.1387667
Fondren, A., Banducci, A. N., Cox, R., & Contractor, A. A. (2022). Processing of Positive Memories Technique (PPMT) among clients reporting traumatic experiences: A case series. Clinical Case Studies, 21, 61-81. https://doi.org/10.1177/15346501211035841
Garcia, H. A., Kelley, L. P., Rentz, T. O., & Lee, S. (2011). Pretreatment predictors of dropout from cognitive behavioral therapy for PTSD in Iraq and Afghanistan war veterans. Psychological Services, 8, 1-11. https://doi.org/10.1037/a0022705
Glaesser, J., Neuner, F., Lütgehetmann, R., Schmidt, R., & Elbert, T., 4(1), 1-6. . (2004). Posttraumatic stress disorder in patients with traumatic brain injury. BMC Psychiatry, 4, 1-6. https://doi.org/10.1186/1471-244X-4-5
Grella, S. L., Fortin, A. H., Ruesch, E., Bladon, J. H., Reynolds, L. F., Gross, A., Shpokayte, M., Cincotta, C., Zaki, Y., & Ramirez, S. (2022). Reactivating hippocampal-mediated memories during reconsolidation to disrupt fear. Nature Communications, 13(1), 1-19. https://doi.org/10.1038/s41467-022-32246-8
Hauer, B. J., Wessel, I., Engelhard, I. M., Peeters, L. L., & Dalgleish, T. (2009). Prepartum autobiographical memory specificity predicts post-traumatic stress symptoms following complicated pregnancy. Memory, 17, 544-556. https://doi.org/10.1080/09658210902953836
Hembree, E. A., Foa, E. B., Dorfan, N. M., Street, G. P., Kowalski, J., & Tu, X. (2003). Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress, 16, 555-562. https://doi.org/10.1023/B:JOTS.0000004078.93012.7d
Hitchcock, C., Werner-Seidler, A., Blackwell, S. E., & Dalgleish, T. (2017). Autobiographical episodic memory-based training for the treatment of mood, anxiety and stress-related disorders: A systematic review and meta-analysis. Clinical Psychology Review, 52, 92-107. https://doi.org/10.1016/j.cpr.2016.12.003
Jacobson, I. G., Southwick, S. M., & Kosten, T. R. (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry, 158, 1184-1190. https://doi.org/10.1176/appi.ajp.158.8.1184
Jobson, L., Cheraghi, S., & Moradi, A. R. (2016). Brief report: Comparing the autobiographical remembering of Iranian immigrant trauma survivors with that of Iranian and British trauma survivors. Applied Cognitive Psychology, 30, 635-642. https://doi.org/10.1002/acp.3230
Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry, 61, 4-12.
Kida, S. (2019). Reconsolidation/destabilization, extinction and forgetting of fear memory as therapeutic targets for PTSD. Psychopharmacology, 236, 49-57. https://doi.org/10.1007/s00213-018-5086-2
Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. Journal of Traumatic Stress, 26, 537-547. https://doi.org/10.1002/jts.21848
Kindt, M., & van Emmerik, A. (2016). New avenues for treating emotional memory disorders: Towards a reconsolidation intervention for posttraumatic stress disorder. Therapeutic Advances in Psychopharmacology, 6, 283-295. https://doi.org/10.1177/2045125316644541
LaGarde, G., Doyon, J., & Brunet, A. (2010). Memory and executive dysfunctions associated with acute posttraumatic stress disorder. Psychiatry Research, 177, 144-149. https://doi.org/10.1016/j.psychres.2009.02.002
Leiner, A. S., Kearns, M. C., Jackson, J. L., Astin, M. C., & Rothbaum, B. O. (2012). Avoidant coping and treatment outcome in rape-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 80, 317-321. https://doi.org/10.1037%2Fa0026814
Magruder, K. M., McLaughlin, K. A., & Elmore Borbon, D. L. (2017). Trauma is a public health issue. European Journal of Psychotraumatology, 8(1375338). https://doi.org/10.1080/20008198.2017.1375338
Matlin, M. W., & Stang, D. J. (1978). The Pollyanna principle: Selectivity in language, memory, and thought. . Schenkman Publishing Company.
Miguel-Alvaro, A., Guillén, A. I., Contractor, A. A., & Crespo, M. (2021). A scoping review of positive memory intervention techniques and models. Memory, 29(6), 1-18. https://doi.org/10.1080/09658211.2021.1937655
Moore, S. A., & Zoellner, L. A. (2007). Overgeneral autobiographical memory and traumatic events: An evaluative review. Psychological Bulletin, 133, 419-437. https://doi.org/10.1037/0033-2909.133.3.419
Moradi, A. R., Piltan, M., Choobin, M. H., Azadfallah, P., Watson, P., Dalgleish, T., & Hitchcock, C. (2021). Proof-of-concept for the autobiographical Memory Flexibility (MemFlex) intervention for Posttraumatic Stress Disorder. Clinical Psychological Science, 9, 686-698. https://doi.org/10.1177/2167702620982576
Ono, M., Devilly, G. J., & Shum, D. H. (2016). A meta-analytic review of overgeneral memory: The role of trauma history, mood, and the presence of posttraumatic stress disorder. Psychological Trauma Theory Research Practice and Policy, 8, 157-164. https://doi.org/10.1037/tra0000027
Özdemir, O., Özdemir, P. G., Boysan, M., & Yilmaz, E. (2015). The relationships between dissociation, attention, and memory dysfunction. Nöro Psikiyatri Arşivi, 52, 36-41.
Pacella, M. L., Hruska, B., & Delahanty, D. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders, 27, 33-46. https://doi.org/10.1016/j.janxdis.2012.08.004
Reese, E., & Fivush, R. (2008). The development of collective remembering. Memory, 16, 201-212. https://doi.org/10.1080/09658210701806516
Riggs, D. S., Byrne, C. A., Weathers, F. W., & Litz, B. T. (1998). The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress, 11, 87-101. https://doi.org/10.1023/A:1024409200155
Ritchie, T., Skowronski, J. J., Hartnett, J., Wells, B., & Walker, W. R. (2009). The fading affect bias in the context of emotion activation level, mood, and personal theories of emotion change. Memory, 17, 428–444. https://doi.org/10.1080/09658210902791665
Rounsaville, B. J., Carroll, K. M., & Onken, L. S. (2001). A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology Science and Practice, 8, 133-142. https://doi.org/10.1093/clipsy.8.2.133
Rytwinski, N. K., Scur, M. D., Feeny, N. C., & Youngstrom, E. A. (2013). The co‐occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta‐analysis. Journal of Traumatic Stress, 26, 299-309. https://doi.org/10.1002/jts.21814
Schnurr, P. P. (2017). Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Current Opinion in Psychology, 14, 56-60. https://doi.org/10.1016/j.copsyc.2016.11.005
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry: Interpersonal and Biological Processes, 71, 134-168. https://doi.org/10.1521/psyc.2008.71.2.134
van Marle, H. (2015). PTSD as a memory disorder. European Journal of Psychotraumatology, 6. https://doi.org/10.3402/ejpt.v6.27633
Walker, W. R., Skowronski, J. J., & Thompson, C. P. (2003). Life is pleasant–and memory helps to keep it that way! Review of General Psychology, 7, 203-210. https://doi.org/10.1037/1089-2680.7.2.203
Wang, Q. (2008). On the cultural constitution of collective memory. Memory, 16, 305-317. https://doi.org/10.1080/09658210701801467
Wang, Q., & Conway, M. A. (2004). The stories we keep: Autobiographical memory in American and Chinese middle-aged adults. Journal of Personality, 72, 911-938. https://doi.org/10.1111/j.0022-3506.2004.00285.x
Wang, Q., & Ross, M. (2007). Culture and memory. In H. Kitayama & D. Cohen (Eds.), Handbook of cultural psychology. (pp. 645-667). Guilford Publications.
Williams, J. M. G., Barnhofer, T., Crane, C., Hermans, D., Raes, F., Watkins, E., & Dalgleish, T. (2007). Autobiographical memory specificity and emotional disorder. Psychological Bulletin, 133, 122-148. https://doi.org/10.1037/0033-2909.133.1.122
Williams, S. E., Ford, J. H., & Kensinger, E. A. (2022). The power of negative and positive episodic memories. Cognitive, Affective, & Behavioral Neuroscience, 22, 869–903. https://doi.org/10.3758/s13415-022-01013-z
Zaragoza Scherman, A., Salgado, S., Shao, Z., & Berntsen, D. (2015a). Event centrality of positive and negative autobiographical memories to identity and life story across cultures. Memory, 23, 1152-1171. https://doi.org/10.1080/09658211.2014.962997
Zaragoza Scherman, A., Salgado, S., Shao, Z., & Berntsen, D. (2015b). Life span distribution and content of positive and negative autobiographical memories across cultures. Psychology of Consciousness: Theory, Research, and Practice, 2, 475–489. https://doi.org/10.1037/cns0000070



