Monitoring patients’ progress and providing therapists with feedback is a powerful tool that can make a significant difference in the effectiveness of psychological treatments. But have you ever wondered why some therapists seem to benefit more from feedback than others? What factors play a role in whether or not feedback leads to better treatment outcomes? To answer these questions, we delve into the fascinating realm of belief updating.
Belief Updating
Imagine you’re a therapist, and you’ve been working with a patient for a while. Based on your clinical experience, you have certain beliefs about how the therapy is progressing. Perhaps you think your patient’s symptoms are improving steadily. Now, you receive (accurate) patient-reported feedback on the actual treatment progress, which may confirm your beliefs (i.e., continued improvement) or challenge them (i.e., discontinuation of improvement). The crucial question is: what determines whether therapists use this feedback to update their beliefs?
Precision Matters
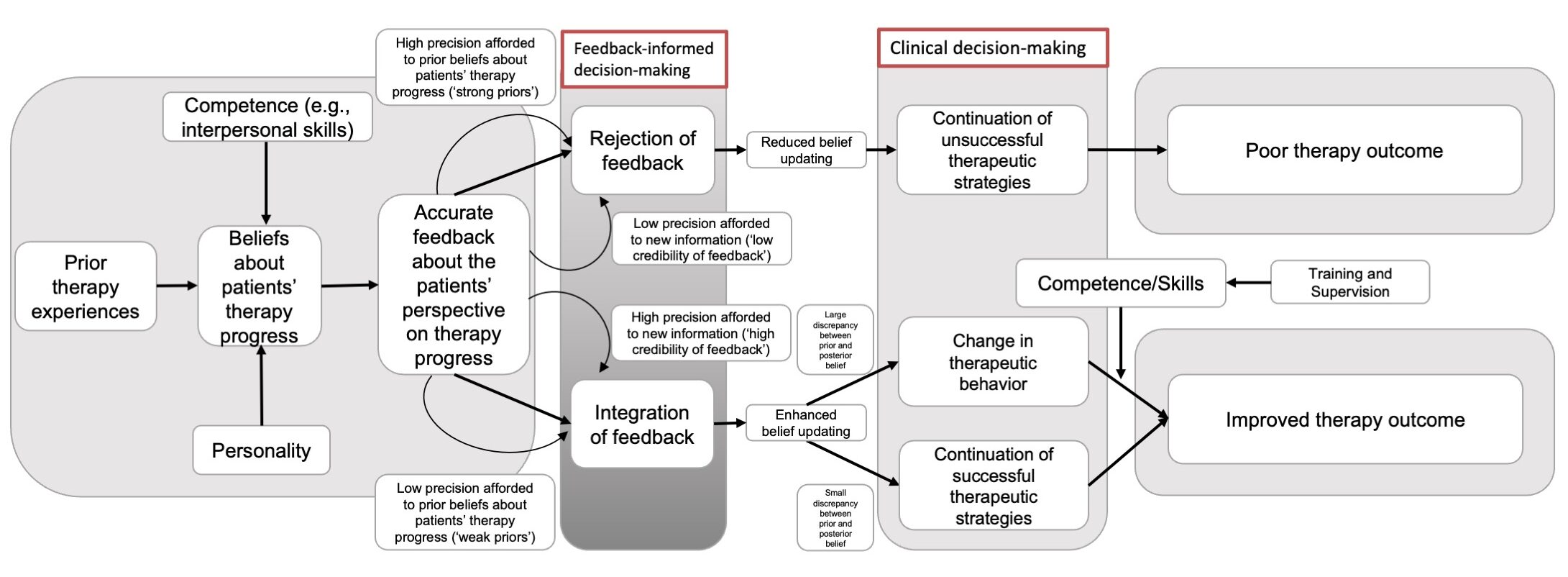
Feedback that is perceived as more precise is more likely to influence therapists’ beliefs. However, humans tend to integrate desirable information provided by feedback more readily than undesirable information. This optimism bias means that therapists may be inclined to accept confirmatory feedback and disregard disconfirmatory feedback, potentially overestimating the success of their therapeutic approach. In fact, whether feedback on treatment progress is integrated into the therapist’s belief system is not only related to the credibility of the feedback itself, but also to therapist’s prior beliefs about the patient’s therapy progress and the confidence afforded to them. Thus, feedback can be rejected in two cases: either high precision is afforded to prior (yet overly optimistic) beliefs about patients’ therapy progress or low precision is afforded to feedback, both increasing the likelihood to hinder belief updating and continuation of (unsuccessful) therapeutic strategies that ultimately lead to poor treatment outcome. We illustrate the belief updating model of feedback-outcome research in Figure 1.
Figure 1.
Clinical and Public Health Implications
The power of feedback in psychological treatments lies in its ability to update beliefs. By understanding how belief updating works, we can enhance clinical training, improve feedback delivery and use, and ultimately, provide more effective therapy. So, what do these insights into belief updating mean precisely for clinical practice?
- Clinical Training: Therapists should be trained to strike a balance between confidence in their ability to judge patient progress (i.e., their own beliefs) and openness to feedback. Considering the trainee’s prior therapy experience, competence level and personality, supervisors can play a crucial role in helping therapists recognize and correct biases, encouraging them to be open to weighing new contradictory evidence provided by feedback. By doing so, we can reduce mismatches in belief systems and increase the predictability and certainty in the therapeutic environment.
- Feedback Delivery: Feedback about patients’ progress should be perceived as accurate (i.e., precise) and come from credible sources. Measurement-based care, where precise empirical evidence can be systematically gathered, could help therapists enhance their understanding of the treatment process. Here, creating a nuanced credibility picture of the feedback system (i.e., strengths and weaknesses) and the information provided (e.g., by providing also confidence intervals of a given score) is key. Moreover, it may help to also collect therapists’ ratings on how they perceived their patients’ progress (before providing the feedback) to be able to confront therapists with the potential discrepancy between their view and that of their patients.
- Feedback Use: Therapists’ beliefs should be reassessed after the provision of feedback. Supervisors can support trainees in whether and how to translate updated beliefs into therapeutic actions. This process of belief updating is essential for using feedback effectively and, ultimately, improving treatment outcomes.
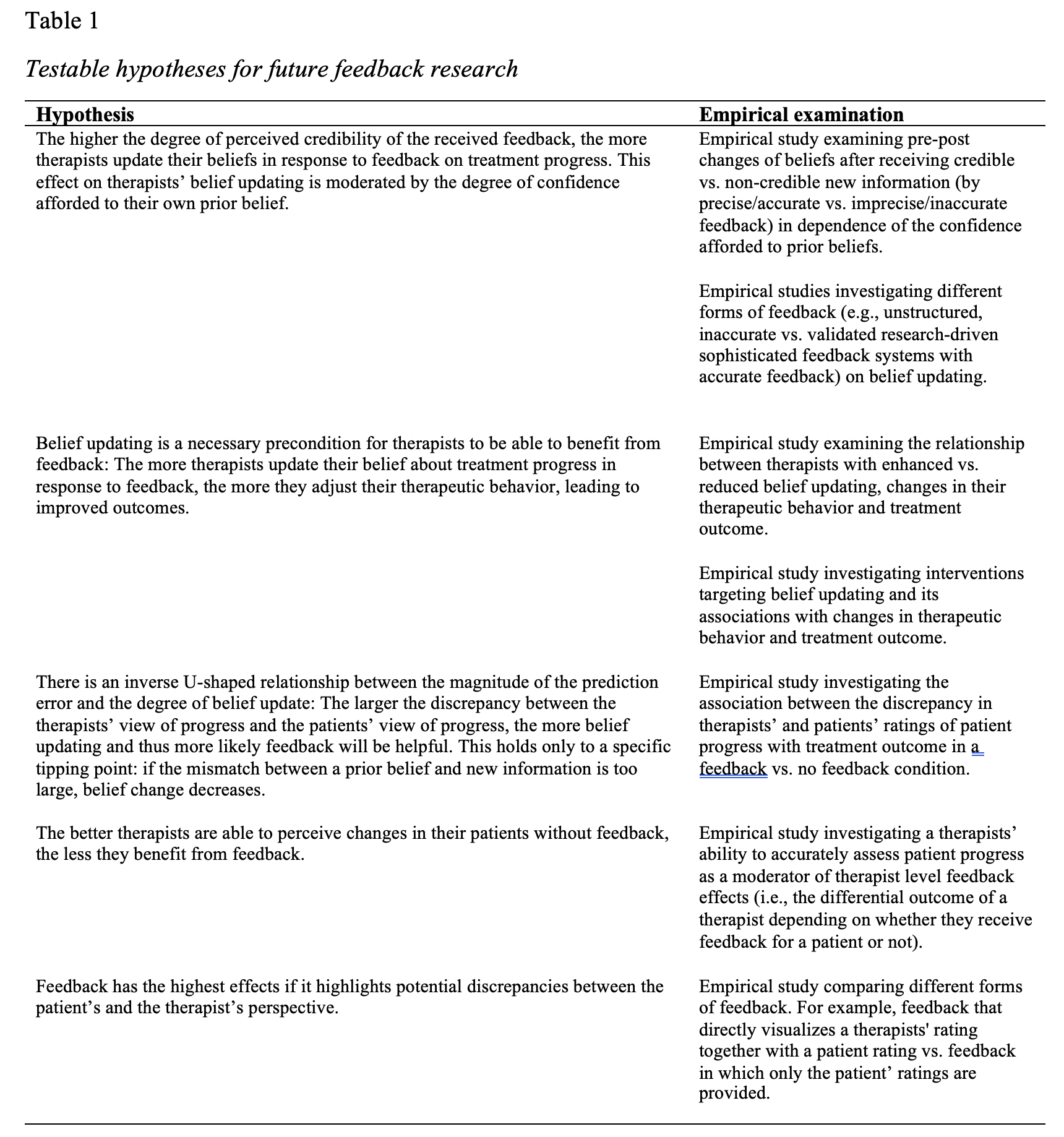
This not only benefits individual patients but also has significant implications for public health, as better therapy outcomes can lead to improved mental health on a larger scale. Belief updating can be a bridge that connects cognitive science to clinical practice, and it’s a bridge we should continue to explore and refine. For this purpose, we provide some future research directions in Table 1.
Target Article
Herzog, P., Kube, T., & Rubel, J. (2023). Why some psychotherapists benefit from feedback on treatment progress more than others: A belief updating perspective. Clinical Psychology: Science and Practice. https://doi.org/10.1037/cps0000174
Discussion Questions
- How can prior beliefs about therapy progress and the degree of precision afforded to them be measured reliably and validly?
- How can the provision of feedback be improved by considering the multidimensional nature of feedback (e.g., symptom change vs. treatment recommendation)?
- How can the accuracy of feedback be increased?
- What credible source of information other than standardized PROM measures (e.g., observer-rated and self-rated data, patients’ qualitative reports, therapist’s notes and observations of patients’ behavior, video-based supervision, previous therapists) should be included in a feedback system?
- How can multiple sources of information be integrated into feedback systems in a way that clinically support the therapist in weighting them against each other?
About the Authors
 Philipp Herzog, PhD, is a postdoctoral researcher and lecturer at the University of Kaiserslautern-Landau (RPTU), currently visiting the Richard J. McNally Lab at the Department of Psychology at Harvard University. Shaped by his clinical experience as a licensed clinical psychologist, he is interested in how to best understand, measure, prevent, and treat complex and severe mental health problems after (repeated) exposure to adverse, extremely threatening life events (e.g., posttraumatic stress disorder), aiming to improve clinical decision-making. Dr. Herzog (https://www.philipp-herzog.com/) can be contacted at [email protected], and you can follow him on Twitter at @herzog_ph.
Philipp Herzog, PhD, is a postdoctoral researcher and lecturer at the University of Kaiserslautern-Landau (RPTU), currently visiting the Richard J. McNally Lab at the Department of Psychology at Harvard University. Shaped by his clinical experience as a licensed clinical psychologist, he is interested in how to best understand, measure, prevent, and treat complex and severe mental health problems after (repeated) exposure to adverse, extremely threatening life events (e.g., posttraumatic stress disorder), aiming to improve clinical decision-making. Dr. Herzog (https://www.philipp-herzog.com/) can be contacted at [email protected], and you can follow him on Twitter at @herzog_ph.
 Tobias Kube, PhD, temporarily holds the Chair for Clinical Psychology and Psychotherapy at the Georg August University of Göttingen, Germany. He is a licensed psychotherapist, trained in cognitive-behavioral therapy. In his research, he investigates how people construe and sustain their subjective reality and how this relates to mental health problems. Dr. Kube can be contacted at [email protected].
Tobias Kube, PhD, temporarily holds the Chair for Clinical Psychology and Psychotherapy at the Georg August University of Göttingen, Germany. He is a licensed psychotherapist, trained in cognitive-behavioral therapy. In his research, he investigates how people construe and sustain their subjective reality and how this relates to mental health problems. Dr. Kube can be contacted at [email protected].
 Julian Rubel, PhD, is a full professor at Osnabrück University and the director of the university’s outpatient research and training clinic for adults. He is a licensed psychotherapist, trained in cognitive-behavioral therapy. In his research, he develops and investigates decision-support tools for clinicians aimed at reducing premature treatment termination and non-response. Prof. Dr. Rubel can be contacted at [email protected], and you can follow him on Twitter at @julian_rubel.
Julian Rubel, PhD, is a full professor at Osnabrück University and the director of the university’s outpatient research and training clinic for adults. He is a licensed psychotherapist, trained in cognitive-behavioral therapy. In his research, he develops and investigates decision-support tools for clinicians aimed at reducing premature treatment termination and non-response. Prof. Dr. Rubel can be contacted at [email protected], and you can follow him on Twitter at @julian_rubel.